Blastomycosis is a fungal infection that often flies under the radar, yet it can mimic common respiratory illnesses like pneumonia. This deceptive nature makes it vital to understand what blastomycosis is and how to recognize its symptoms. Originating from a fungus found in moist soil and decaying organic matter, this illness poses risks, especially for those living in certain regions of North America.
As we delve into the intricacies of blastomycosis, you’ll learn about its transmission paths, potential complications, and treatment options. Whether you’re seeking information for yourself or a loved one, gaining insight into this condition can make all the difference. Join us as we explore each aspect of blastomycosis—knowledge is your best defense against this hidden threat!
What is Blastomycosis? A Clear Explanation
Blastomycosis is a fungal infection caused by the Blastomyces dermatitidis fungus. This organism thrives in moist environments, often found in soil and decaying wood.
When inhaled, spores can enter the lungs, leading to respiratory issues that may resemble pneumonia. The body’s immune response may contain the infection initially; however, it can spread beyond the lungs if not treated promptly.
This disease primarily affects individuals residing in specific areas of North America, particularly near lakes or riverbanks where the spores are more prevalent.
“What is EBV’s Impact on Your Throat? Understanding Epstein-Barr”
While anyone can contract blastomycosis, certain factors increase susceptibility—like weakened immune systems or exposure to contaminated environments. Understanding this infection’s origins helps underscore its potential dangers and emphasizes why awareness is crucial for at-risk populations.
Recognizing Blastomycosis Symptoms: From Mild to Severe
Blastomycosis symptoms can vary widely, ranging from mild to severe. Early signs often mimic those of a respiratory infection. Patients might experience cough, fever, and chest pain.
As the disease progresses, symptoms may intensify. Night sweats and weight loss are commonly reported in more advanced cases. Fatigue can become debilitating as well.
Some individuals may develop skin lesions that are characteristic of blastomycosis. These lesions typically appear as raised bumps or ulcers on various body parts.
“Could It Be Kawasaki Disease? Critical Signs in Children”
In rare instances, the fungus spreads beyond the lungs to other organs like bones or the central nervous system. Neurological symptoms such as confusion or headaches could arise if this occurs.
Recognizing these signs early is crucial for effective treatment. If you notice any concerning symptoms after exposure to endemic areas, seeking medical attention is vital for proper diagnosis and care.
How Blastomycosis Spreads: Understanding Fungal Transmission
Blastomycosis is caused by the fungus *Blastomyces dermatitidis*, which thrives in moist soil and decaying organic matter. The primary mode of transmission to humans occurs through inhalation of airborne spores.
Activities that disturb soil, such as digging or construction, can release these spores into the air. Once inhaled, they travel to the lungs where they can begin to cause infection.
“What Are the Early Signs of Esophageal Cancer? Complete Guide”
In some cases, individuals may also contract blastomycosis through direct contact with contaminated materials like wood or animal remains. However, this route is less common than respiratory exposure.
Geographically, certain regions—particularly near water bodies in North America—are more prone to outbreaks. Awareness of environmental conditions is crucial for reducing risk and protecting vulnerable populations from potential infections.
Diagnosing Blastomycosis: Tests Your Doctor May Recommend
Diagnosing blastomycosis involves a series of tests to confirm the presence of the fungus. Your doctor may start with a detailed medical history and physical examination. This helps identify symptoms that resemble pneumonia or other respiratory illnesses.
“Why Does Angioedema Cause Throat Swelling? Expert Explanation”
Laboratory tests play a crucial role in diagnosis. A sputum sample may be collected to check for fungal elements under a microscope. Blood tests can also detect antibodies produced in response to the infection.
Imaging studies, such as chest X-rays or CT scans, help visualize lung involvement and potentially reveal lesions associated with blastomycosis. In some cases, biopsy of affected tissue might be necessary for definitive diagnosis.
Timely diagnosis is essential for effective treatment. If you present symptoms consistent with this fungal infection, discussing these testing options with your healthcare provider is vital for accurate identification and management of blastomycosis.
Treatment Options for Blastomycosis: Antifungal Medications and More
Treating blastomycosis primarily involves antifungal medications. Itraconazole and amphotericin B are the most common options prescribed by healthcare providers.
Itraconazole is typically used for mild to moderate cases. Patients usually take it orally, making it a convenient choice for long-term management. The treatment course can last several months, depending on individual responses.
“How Long Does Laryngitis Last? Recovery Timeline & Treatment”
For severe or disseminated infections, amphotericin B is often recommended. This potent medication may require intravenous administration in a hospital setting due to potential side effects.
In some instances, corticosteroids might be added to reduce inflammation in the lungs, especially when breathing difficulties occur. However, this approach needs careful consideration since steroids can suppress immune function.
Monitoring progress through follow-up appointments is crucial during treatment. Regular assessments help ensure that the fungal infection is responding appropriately to therapy.
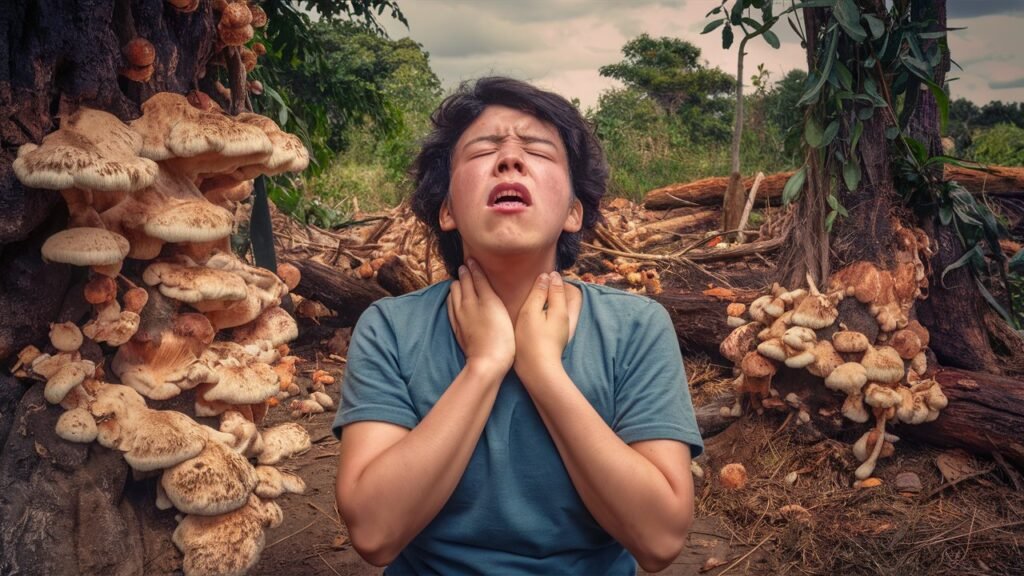
Can Blastomycosis Affect Your Throat? Understanding Oral Symptoms
Blastomycosis primarily affects the lungs, but it can also manifest in other areas of the body, including the throat. When this fungal infection spreads beyond the respiratory system, it may lead to oral symptoms.
“What is Mycoplasma Pneumoniae’s Effect on Your Throat?”
Individuals might experience a sore throat or discomfort while swallowing. These symptoms can mimic those seen in viral infections or bacterial illnesses, making diagnosis more challenging.
In some cases, lesions may develop in the mouth or throat region. This occurs when the fungus proliferates and causes inflammation. Such lesions can result in pain and difficulty eating.
It’s essential to be aware of these potential manifestations if you are at risk for blastomycosis. Early recognition plays a crucial role in effective treatment and recovery from this complex infection. Always consult healthcare professionals if you notice unusual symptoms affecting your throat or mouth area.
Blastomycosis vs Bacterial Pneumonia: Spotting the Differences
Blastomycosis and bacterial pneumonia share some symptoms, making differentiation crucial. Both can cause cough, fever, and chest pain. However, their origins are starkly different.
Blastomycosis is a fungal infection typically contracted from inhaling spores found in soil or decaying organic material. In contrast, bacterial pneumonia arises from bacteria affecting the lungs, often following a cold or flu.
Diagnosis relies on specific tests. A culture of sputum may reveal fungi for blastomycosis while bacterial infections usually show distinct types of bacteria under microscopic examination.
“How Does Secondary Syphilis Affect Your Throat? Key Information”
Treatment varies significantly as well; antifungal medications are necessary for blastomycosis whereas antibiotics address bacterial pneumonia effectively.
Understanding these differences plays a vital role in ensuring proper treatment and recovery outcomes for affected individuals. Being aware of exposure history can also guide patients on when to seek medical attention if symptoms develop.
Complications of Untreated Blastomycosis: What You Need to Know
Untreated blastomycosis can lead to serious complications. The most common issues arise when the infection spreads beyond the lungs. This can result in chronic respiratory problems, making it difficult to breathe and engage in daily activities.
In severe cases, blastomycosis may affect other organs such as the skin, bones, or central nervous system. Skin lesions can develop, leading to painful sores that require medical intervention.
Neurological symptoms might emerge if the fungus reaches the brain or spinal cord. These include headaches, confusion, and even seizures.
Long-term consequences of untreated infections often involve permanent damage to lung tissues. This irreversible harm may necessitate ongoing treatment for respiratory conditions similar to COPD or asthma.
Being aware of these potential complications underscores the importance of early diagnosis and effective treatment for anyone suspected of having blastomycosis.
Blastomycosis in Different Body Systems: Beyond the Lungs
Blastomycosis primarily targets the lungs, but its effects can extend to various body systems. When the fungal spores enter the bloodstream, they may disseminate to other organs and tissues.
Skin involvement is common. Patients might develop lesions that range from superficial ulcers to deeper abscesses. These manifestations can be painful and often resemble other skin conditions.
“What is Blastomycosis? Understanding Throat Symptoms”
The central nervous system is not immune either. Rare cases of meningitis have been reported, leading to symptoms like headaches, confusion, or seizures.
Bone infections are also possible. Blastomyces can invade bones, causing osteomyelitis which results in localized pain and swelling.
In severe situations, it may affect the genitourinary system as well. Symptoms could include urinary issues or discomfort during urination.
Recognizing these extra-pulmonary symptoms early is crucial for effective treatment and recovery.
Who’s at Risk for Blastomycosis? Understanding Vulnerable Populations
Certain groups of people are more susceptible to blastomycosis. Individuals with weakened immune systems face a higher risk. This includes those living with HIV/AIDS, cancer patients undergoing chemotherapy, and organ transplant recipients.
Men aged 50 years and older also represent a vulnerable population. Factors such as occupational exposure can increase their likelihood of contracting the infection. Jobs involving outdoor activities or working in woods may elevate this risk.
Additionally, individuals who engage in recreational activities like camping or hunting in endemic areas should exercise caution. The fungi thrive in specific environments, particularly near bodies of water and decaying organic matter.
Pregnant women may experience changes that affect their immune response, making them more prone to infections like blastomycosis. Awareness is key for anyone falling into these categories to take preventive measures seriously when spending time outdoors.
Preventing Blastomycosis: Tips for Those in Endemic Areas
Preventing blastomycosis is crucial for those living in endemic areas. Awareness of the environment can significantly reduce your risk.
First, avoid activities that disturb soil or dust, especially in wooded or wet regions. This includes digging, gardening, or exploring areas with decaying vegetation.
When outdoors, wear protective clothing such as gloves and masks to limit exposure. Opt for long sleeves and pants to shield your skin while hiking or working near potential habitats for the fungus.
Be cautious during flood events. Blastomyces dermatitidis thrives in moist conditions, increasing the likelihood of exposure when flooding occurs.
Regularly inspect pets and livestock for signs of respiratory distress. Animals can also contract blastomycosis and may spread spores around your home.
Educating yourself about local health advisories can further enhance your prevention strategies. Stay informed about outbreaks to better prepare yourself against this fungal infection.
Living with Blastomycosis: Coping with Diagnosis and Treatment
Living with Blastomycosis can be a challenging experience, both physically and emotionally. The diagnosis often brings uncertainty and anxiety. It’s crucial to seek support from loved ones or support groups who understand the journey.
Treatment typically involves antifungal medications, which may lead to side effects like fatigue or nausea. Staying informed about your treatment plan can empower you during this time. Regular check-ins with healthcare providers are essential for monitoring progress.
Adopting a healthy lifestyle plays a significant role in recovery. A balanced diet rich in nutrients supports the immune system, while gentle exercise can enhance overall well-being.
Mindfulness practices such as yoga or meditation may help manage stress levels associated with living with a chronic condition. Remember that every individual’s journey is unique; sharing experiences might foster connections that provide comfort and encouragement along the way.
Blastomycosis and Your Immune System: A Complex Relationship
Blastomycosis is a fungal infection that poses unique challenges to the immune system. When exposed, the fungus can evade detection and thrive in individuals with compromised immunity.
Healthy immune systems typically recognize and fight off pathogens effectively. However, Blastomyces dermatitidis, the causative agent of blastomycosis, has developed strategies to avoid being eliminated. It can transform into a yeast form within human tissues, making it more resilient against immune responses.
People with weakened immune systems—such as those living with HIV/AIDS or undergoing immunosuppressive therapies—are particularly vulnerable. Their bodies may struggle to mount an adequate defense against this opportunistic pathogen.
Interestingly, even healthy individuals can become infected if they encounter high levels of spores in endemic areas. This highlights how environmental factors and individual health intersect when dealing with blastomycosis.
Can Blastomycosis Recur? Understanding Reinfection Risks
Blastomycosis can indeed recur after initial treatment. This fungal infection, caused by the Blastomyces dermatitidis organism, has a unique way of interacting with the immune system.
Once a person is infected and treated successfully, they may develop some level of immunity. However, this immunity isn’t foolproof. Factors like weakened immune systems or environmental exposure can increase the risk of reinfection.
Living in or traveling to endemic areas also plays a role in recurrence. The spores are present in soil and decaying organic matter, making certain regions more susceptible for those who have previously battled blastomycosis.
It’s essential to monitor your health if you’ve had blastomycosis before. Any new respiratory symptoms should prompt immediate medical attention for proper evaluation and management. Being proactive about your health helps mitigate risks associated with potential reinfection.
Blastomycosis in Pets: What Pet Owners Should Know
Blastomycosis can affect pets, especially dogs. The disease is caused by the same fungus that impacts humans. Pets can contract this infection after inhaling spores found in moist soil or decaying organic matter.
Symptoms in animals may vary but often include coughing, lethargy, weight loss, and fever. Skin lesions are also common in affected pets. If you notice these signs, seek veterinary care promptly.
Diagnosis usually involves a combination of physical exams and laboratory tests to identify the fungus. Treatment typically requires antifungal medications tailored for your pet’s needs.
Prevention is crucial since blastomycosis thrives in specific environments. Avoid letting your dog roam freely in areas known as endemic regions during high-risk seasons.
Always keep an eye on your pet’s behavior and health changes. Early detection plays a key role in successful treatment outcomes for our furry friends facing this fungal challenge.
Recovery Time for Blastomycosis: Setting Realistic Expectations
Recovery time for blastomycosis varies significantly among individuals. Typically, patients may start to feel better within a few weeks of starting antifungal treatment. However, complete recovery can take several months.
Factors influencing recovery include the severity of the infection and the patient’s overall health. Those with weakened immune systems might experience prolonged symptoms or complications, extending their healing period.
Regular follow-up appointments are essential to monitor progress and adjust treatments if necessary. Some patients may require extended therapy lasting six months or more.
Staying hydrated and maintaining a balanced diet can support recovery efforts. Additionally, getting adequate rest is crucial for your body’s healing process.
Being patient is key during this time. The body needs time to heal fully from such an invasive fungal infection like blastomycosis.
When to Seek Medical Help for Suspected Blastomycosis
If you suspect blastomycosis, it’s crucial to seek medical help promptly. Early intervention can significantly impact your recovery.
Watch for symptoms such as persistent cough, fever, or chest pain. These signs may initially feel like common respiratory infections but can escalate quickly. If these symptoms persist beyond a week, don’t hesitate to consult a healthcare professional.
Individuals with weakened immune systems or chronic illnesses should be especially vigilant. They are at higher risk of severe complications and need swift evaluation if they experience any related symptoms.
Moreover, if you’ve been in an area known for fungal exposure—such as wetland regions leading to potential blastomycosis infection—it’s wise to discuss this with your doctor even before symptoms appear.
Remember that timely diagnosis is critical for effective treatment options. Don’t ignore unusual health changes; seeking medical advice could make all the difference in managing this infection effectively.
Blastomycosis Research: New Discoveries and Future Treatments
Recent research on blastomycosis has gained momentum, focusing on better understanding the pathogen and its effects. Scientists are investigating genetic factors that allow Blastomyces dermatitidis to thrive in certain environments. This knowledge could lead to targeted prevention strategies.
Innovative treatment approaches are also being explored. Researchers are assessing new antifungal compounds that may be more effective than traditional therapies. These alternatives aim to reduce side effects and improve patient outcomes.
In addition, studies into vaccine development show promise. A vaccine could provide immunity for at-risk populations, significantly reducing infection rates.
The role of climate change is under scrutiny as well. Understanding how environmental shifts influence fungal growth patterns is crucial for anticipating outbreaks in endemic areas.
Collaboration among researchers worldwide enhances these efforts, paving the way for advancements in diagnosing and treating this challenging disease effectively.
The Impact of Climate Change on Blastomycosis Spread
Climate change is increasingly recognized as a significant factor influencing the spread of various infectious diseases, including blastomycosis. As temperatures rise and weather patterns shift, regions that were previously unsuitable for the fungus *Blastomyces dermatitidis* may become more conducive to its growth and transmission.
Warmer climates can prolong the fungal life cycle while also impacting soil moisture levels, promoting conditions where spores thrive. This means areas that once had low incidences of blastomycosis might see an influx of cases as the fungus finds new grounds to colonize.
Additionally, increased rainfall and flooding are likely to disturb soil ecosystems, releasing dormant spores into the air. These changes heighten exposure risks for people working or spending time outdoors in endemic areas.
As habitats shift due to climate fluctuations, vulnerable populations—such as those with weakened immune systems—face greater susceptibility to this infection. Awareness of these dynamics is crucial for public health efforts aimed at preventing outbreaks in emerging hotspots.
Monitoring ecological shifts will be essential in predicting future trends related to blastomycosis prevalence. By understanding how environmental factors contribute to disease spread, we can take proactive measures not only for human health but also when addressing potential impacts on pets and wildlife affected by this fungal infection.


