Lemierre’s Syndrome might not be a term you hear every day, but it’s a condition that demands attention. Often overshadowed by more common illnesses, this rare disease can have serious implications following what seems like an ordinary sore throat. Understanding the nuances of Lemierre’s Syndrome is crucial for anyone who has ever experienced lingering throat pain or other unusual symptoms.
This blog post will guide you through everything you need to know about Lemierre’s Syndrome and its connection to sore throats. From identifying key symptoms to understanding how it’s diagnosed and treated, we’ll cover all bases for your peace of mind. Whether you’re a healthcare professional, a concerned parent, or simply someone wanting to expand their medical knowledge, this article aims to shed light on what could easily be deemed “the forgotten disease.” Join us as we explore this critical topic in detail!

What is Lemierre’s Syndrome? Understanding the Basics
Lemierre’s Syndrome is a rare but severe condition that typically follows a throat infection. It often begins with symptoms like sore throat, fever, and difficulty swallowing.
This syndrome occurs when bacteria from the throat invade nearby structures, leading to thrombophlebitis of the internal jugular vein. The most common culprit is Fusobacterium necrophorum, a type of anaerobic bacteria.
“Is It Flu or Just a Sore Throat? How to Tell the Difference”
As the infection spreads, it can lead to serious complications such as septic emboli—fragments of infected tissue and pus that travel through the bloodstream. These can lodge in organs like the lungs or heart.
Though Lemierre’s Syndrome may sound alarming, early recognition and treatment significantly improve outcomes. Awareness is crucial since many healthcare providers might overlook it due to its rarity compared to other infections. Understanding this disease empowers patients and caregivers alike to seek timely medical assistance when necessary.
Recognizing the Symptoms of Lemierre’s Syndrome
Lemierre’s Syndrome often begins with a seemingly harmless sore throat. However, as the infection progresses, symptoms become more severe and alarming.
Patients may develop high fevers and chills. These signs indicate that something is wrong beyond a typical throat infection.
“When Should You Worry About Tonsillitis? Expert Advice”
Swelling in the neck can occur due to infected blood clots. This swelling might cause pain or discomfort when swallowing.
You may also notice unusual fatigue or weakness. Such symptoms suggest that your body is fighting an aggressive infection.
In some cases, individuals experience respiratory issues like difficulty breathing or chest pain. These are serious indicators of potential complications arising from Lemierre’s Syndrome.
Headaches and ear pain are additional symptoms that could point toward this rare condition. Recognizing these signs early can make all the difference in treatment outcomes and recovery time.
Causes of Lemierre’s Syndrome: From Sore Throat to Serious Infection
Lemierre’s Syndrome often begins with a common sore throat. This seemingly innocuous symptom can escalate into something far more severe.
The primary culprit is usually an infection in the throat, often triggered by bacteria like Fusobacterium necrophorum. These bacteria are part of the normal flora but can become pathogenic under certain conditions.
“Can Dry Air Damage Your Throat? Prevention & Treatment Guide”
Once they invade the tissues, they may lead to thrombophlebitis—a clot formation in the internal jugular vein. This complication allows bacteria to enter the bloodstream, spreading infection throughout the body.
Poor dental hygiene or recent viral infections can also increase susceptibility. In some cases, young adults and teenagers tend to be at higher risk due to their lifestyle choices and overall health status.
Understanding these causes is crucial for early detection and intervention before serious complications arise.
How Doctors Diagnose Lemierre’s Syndrome: Tests and Procedures
Diagnosing Lemierre’s Syndrome requires a careful approach due to its complexity. Doctors start by taking a thorough medical history and performing a physical examination. They pay close attention to symptoms such as sore throat, fever, and swelling in the neck.
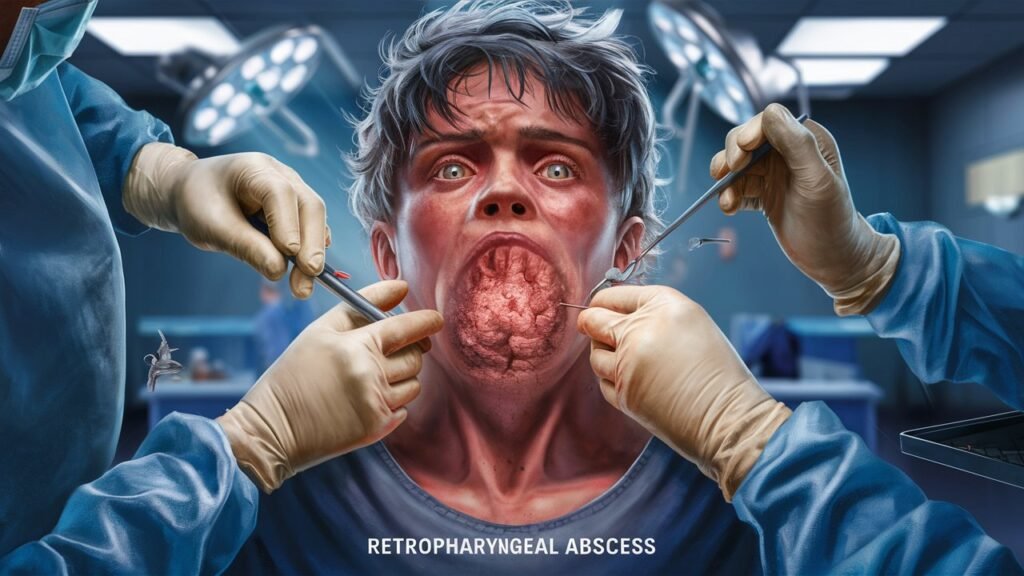
“What is a Peritonsillar Abscess? Emergency Signs to Watch”
Blood tests play a crucial role in the diagnosis. Elevated white blood cell counts can indicate an infection. Cultures may also be taken to identify specific bacteria responsible for the condition.
Imaging tests are essential for assessing complications. Ultrasound or CT scans help visualize any abscesses or clots related to the infection. These images guide treatment decisions and assess severity.
If necessary, doctors may perform additional procedures like endoscopy to examine affected areas closely. Each step is critical in confirming Lemierre’s Syndrome while ruling out other potential conditions that mimic its symptoms.
Treatment Options for Lemierre’s Syndrome: Antibiotics and More
The primary treatment for Lemierre’s syndrome is the use of antibiotics. These powerful medications target the bacteria responsible for the infection, often starting with broad-spectrum options like piperacillin-tazobactam or ceftriaxone.
“How to Identify Oral Thrush? Complete Guide to Candidiasis”
In severe cases, intravenous (IV) antibiotics may be required. This allows for a higher concentration in the bloodstream and ensures rapid action against the infection. Treatment duration can vary but typically lasts several weeks to ensure complete resolution.
Alongside antibiotics, supportive care plays a critical role. Patients may require fluids and pain management to address symptoms like fever and discomfort.
Surgery might also come into play if there are abscesses that need drainage or if there’s vascular compromise due to clot formation in veins affected by the infection. Close monitoring is essential throughout this process to manage any potential complications effectively.
Complications of Lemierre’s Syndrome: What Can Go Wrong
Lemierre’s Syndrome can lead to serious complications that pose significant health risks. One of the primary concerns is septic thrombophlebitis, where blood clots form in veins due to infection. This condition can result in severe pain and swelling.
Another potential complication is septic emboli. These are small pieces of infected material that can travel through the bloodstream, causing blockages in various organs like the lungs or brain. Symptoms may include sudden chest pain or neurological issues.
In some cases, patients may experience organ failure if critical systems become overwhelmed by infection. The risk of lung abscesses also increases as bacteria spread from the throat to the respiratory system.
Moreover, Lemierre’s Syndrome might trigger other infections throughout the body. Timely medical intervention is crucial to mitigate these dangers and improve outcomes for those affected by this rare disease.
Recovery from Lemierre’s Syndrome: What to Expect
Recovering from Lemierre’s Syndrome can be a lengthy process. After receiving treatment, many patients face a gradual return to health.
Initially, hospitalization is often necessary for close monitoring. Intravenous antibiotics are commonly administered to combat the infection effectively. This intense phase usually lasts several days.
Once stabilized, transitioning to oral antibiotics begins. Patients may experience fatigue and weakness during this time. These symptoms are normal as the body heals.
Follow-up appointments with healthcare providers are essential for tracking recovery progress. Blood tests or imaging studies might be conducted to ensure no complications arise.
Supportive care also plays a crucial role in recovery. Staying hydrated and maintaining proper nutrition helps rebuild strength.
Emotional well-being should not be overlooked either; some individuals may need counseling or support groups as they navigate their healing journey after such an alarming illness.
Can Lemierre’s Syndrome Be Prevented? Understanding Risk Factors
Preventing Lemierre’s Syndrome primarily revolves around addressing its risk factors. One significant factor is the presence of bacterial infections, especially those related to the throat. Timely treatment of conditions like pharyngitis or tonsillitis can reduce the likelihood of complications.
Maintaining good oral hygiene is vital as well. Poor dental health can increase susceptibility to infections that may lead to this syndrome. Regular dental check-ups and proper brushing habits play a crucial role in prevention.
Another important aspect involves understanding individual health status. Those with weakened immune systems or chronic illnesses should take extra precautions during flu seasons or outbreaks of respiratory infections.
Awareness is key; recognizing symptoms early and seeking prompt medical care can prevent severe outcomes associated with Lemierre’s Syndrome. A proactive approach to one’s health significantly lowers risks linked to this rare condition.
Lemierre’s Syndrome vs. Other Throat Infections: Key Differences
Lemierre’s Syndrome often gets confused with more common throat infections like strep throat or tonsillitis. However, there are significant differences that set them apart.
Strep throat is primarily caused by a bacterial infection and usually responds well to antibiotics. Symptoms include a sudden sore throat, fever, and swollen lymph nodes. In contrast, Lemierre’s Syndrome can develop as a complication of an untreated sore throat.
Unlike typical throat infections, Lemierre’s involves the formation of blood clots in the jugular vein due to bacteria entering the bloodstream. This can lead to serious complications like septic thrombophlebitis.
Patients with Lemierre’s may experience additional symptoms such as chest pain or difficulty breathing—signs that indicate a far more severe condition than usual viral or bacterial pharyngitis. Recognizing these distinctions early on is vital for appropriate treatment and management of this rare syndrome.
The History of Lemierre’s Syndrome: Why It’s Called the “Forgotten Disease”
Lemierre’s Syndrome was first identified in 1900 by French physician André Lemierre. He described a rare condition that followed an ordinary throat infection, leading to serious complications like septic thrombophlebitis.
For decades, it remained largely under the radar. With advances in antibiotics and improved medical care, cases became infrequent. Many healthcare professionals started dismissing it as a relic of the past.
This lack of awareness contributed to its “forgotten” label. Medical literature often centers on more common conditions, leaving Lemierre’s Syndrome overshadowed despite its potential severity.
Recent years have seen a resurgence in interest due to rising cases and antibiotic resistance. As healthcare providers become more vigilant about unusual infections, understanding this syndrome is crucial for timely diagnosis and treatment. Recognizing its history helps illuminate why it’s essential not to overlook such potentially dangerous diseases today.
Lemierre’s Syndrome in Young Adults: Why They’re at Higher Risk
Lemierre’s Syndrome predominantly affects young adults, particularly those aged 16 to 30. A combination of factors contributes to this heightened risk.
First, the syndrome often arises from a throat infection, which is more common in younger populations. Viral and bacterial infections can spread quickly among peers, especially in close-contact environments like schools or universities.
Additionally, lifestyle choices play a role. Young adults may engage in behaviors that compromise their immune systems—such as irregular sleep patterns and high-stress levels—making them more susceptible to infections.
Furthermore, certain activities like smoking increase the likelihood of developing respiratory issues and subsequent complications. This creates an environment where bacteria can flourish.
Understanding these risks is crucial for prevention and early identification of symptoms associated with Lemierre’s Syndrome in this age group. Awareness can lead to faster treatment outcomes and better health overall.
Long-term Effects of Lemierre’s Syndrome: What We Know
Lemierre’s Syndrome can leave lasting impacts, particularly concerning the vascular system. The most common long-term effect is persistent fatigue and malaise, which can linger for months after recovery.
Patients may also experience complications related to blood clots. These could lead to issues such as pulmonary embolism or other cardiovascular problems requiring ongoing medical attention.
Neurological effects are another concern. Some individuals report headaches or cognitive difficulties that persist well beyond the acute phase of the illness.
In rare cases, patients develop chronic pain syndromes. This might stem from nerve damage or changes in circulation due to previous infections.
Monitoring by healthcare providers is essential during recovery. Regular follow-ups help manage any emerging symptoms and ensure overall health stability after the syndrome has resolved.
Lemierre’s Syndrome and Antibiotic Resistance: A Growing Concern
Lemierre’s Syndrome often follows a throat infection, typically from bacteria like Fusobacterium necrophorum. Understanding the role of antibiotics in treating this condition is crucial. Unfortunately, increasing antibiotic resistance poses significant challenges.
Many strains of bacteria are becoming resistant to commonly prescribed antibiotics. This resistance can delay treatment and worsen outcomes for patients with Lemierre’s Syndrome. When standard treatments fail, doctors may need to resort to stronger medications or combinations that can have more side effects.
Awareness is key. Patients must be informed about the importance of completing prescribed antibiotic courses. Misuse or overuse contributes heavily to the growing issue of resistance.
Healthcare providers also play a critical role by using judicious prescribing practices and monitoring bacterial sensitivity patterns. The battle against antibiotic-resistant infections requires teamwork between patients and medical professionals to ensure effective treatment strategies remain viable for severe conditions like Lemierre’s Syndrome.
The Role of Imaging in Diagnosing Lemierre’s Syndrome
Imaging plays a crucial role in diagnosing Lemierre’s Syndrome, particularly when symptoms are vague or mimic other conditions. Physicians often rely on imaging techniques to confirm the presence of thrombosis, which is key for this syndrome.
Ultrasound is frequently used as an initial assessment tool. It can effectively visualize blood clots in the internal jugular vein. This non-invasive method helps doctors evaluate abnormalities without subjecting patients to radiation.
CT scans also offer detailed images of neck structures and surrounding tissues. They provide insight into potential abscesses that might be forming due to the infection.
In some cases, MRI may be employed for its superior soft tissue contrast. This helps identify complications that could arise from severe infections.
These imaging modalities assist healthcare providers in making timely decisions about treatment plans tailored specifically for each patient’s needs.
Supportive Care for Patients with Lemierre’s Syndrome
Supportive care plays a crucial role in the management of Lemierre’s Syndrome. Patients often experience severe symptoms that require close monitoring and assistance.
Hydration is essential. Fluids help maintain kidney function and prevent complications related to dehydration. Intravenous fluids may be necessary for those unable to drink adequately.
Pain management should not be overlooked. Analgesics can provide relief from throat pain and general discomfort, making it easier for patients to eat and rest.
Nutritional support is vital as well. Soft foods or enteral feeding may be recommended if swallowing becomes difficult due to throat swelling or pain.
Additionally, emotional support is important. The diagnosis might induce anxiety; counseling and reassurance can significantly improve psychological well-being during recovery.
Comprehensive supportive care enhances patient comfort while addressing various needs throughout the treatment journey.
Rare Complications of Lemierre’s Syndrome: Beyond the Typical Cases
Lemierre’s Syndrome can lead to complications that extend beyond the well-known venous thrombosis and septic emboli. One rare but serious complication is jugular vein thrombosis, which can cause swelling in the neck and difficulty swallowing. This may mimic other throat issues, complicating diagnosis.
Another alarming risk is pulmonary embolism. As infected clots travel to the lungs, patients may experience sudden shortness of breath or chest pain.
Neurological complications are also possible; septic emboli can reach the brain, potentially resulting in strokes or abscesses that require immediate attention.
Additionally, Lemierre’s Syndrome might trigger organ dysfunction due to widespread infection. The kidneys and liver could be affected significantly if sepsis develops.
These rare complications highlight the need for prompt medical intervention when symptoms arise. Early recognition plays a crucial role in reducing risks associated with this condition.
When to Seek Emergency Care: Red Flags for Lemierre’s Syndrome
When it comes to Lemierre’s Syndrome, recognizing the signs early can be crucial. If you experience a sore throat that suddenly worsens, accompanied by fever, chills, or swelling in your neck, it’s important to seek medical attention promptly. Other warning symptoms include difficulty swallowing or breathing and unusual fatigue.
Pay close attention if you notice any redness or swelling around your tonsils and persistent pain that doesn’t improve with standard treatments. Additionally, if you develop sudden chest pain or shortness of breath—especially after experiencing throat issues—these could signal a serious complication related to Lemierre’s Syndrome.
Don’t hesitate to reach out for emergency care if these red flags arise. Timely intervention can make all the difference in managing this condition effectively and preventing severe complications. Awareness is key; being informed about these critical signs not only helps protect yourself but also aids healthcare professionals in providing swift treatment when needed.